The GATeway to treating neurological disorders

One of the smallest protein structures ever determined using cryo-EM, GAT1 is fundamental to GABA neurotransmission and its structural determination is pivotal to developing therapies for a range of GABA-associated neurological disorders.
A cryo-electron microscopy (EM) study led by Cornelius Gati at the University of Southern California Dornsife (CA, USA) has elucidated the atomic structure of the gamma-amino butyric acid (GABA) transporter 1 (GAT1), a vital transmembrane protein for neurotransmission. Knowing GAT1’s structure may enable the development of future treatments for disorders including epilepsy, bipolar disorder, schizophrenia, Parkinson’s and Huntington’s diseases, anxiety and autism spectrum disorder.
GABA is one of the most prevalent neurotransmitters in the brain and functions to inhibit the activity of the receiving neurons. When there is insufficient transmission of GABA, neurons can be overstimulated, leading to seizures and epileptic symptoms.
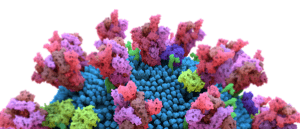 Cryo-EM analysis reveals Omicron’s strong bond with human cells
Cryo-EM analysis reveals Omicron’s strong bond with human cells
The first molecular-level analysis of Omicron’s spike protein reveals mutation-induced chemical bonds are behind the new SARS-CoV-2 variant’s increased transmissibility and antibody evasion.
GAT1 functions to transport extracellular GABA, released during transmission, from the synaptic cleft back into the neuron. An existing treatment for epilepsy is the targeted inhibition of GAT1 with drugs such as tiagabine, which increases the level of GABA in the synaptic cleft and reduces the severity of symptoms.
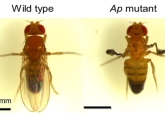
Even though tiagabine is an established therapy, we have previously lacked the mechanistic understanding of its precise interaction with GAT1. To examine the binding interaction between tiagabine and GAT1, Gati’s team utilized cryo-EM of a full-length wild type GAT1 in complex with tiagabine.
“Previous understanding of the inhibitor (tiagabine) was purely based on biochemical studies, which do not provide any details at the atomic scale,” explained Gati. “We can now pinpoint specific parts of the drug that interact with the protein.”
The insight provided by Gati illuminates the previously unknown mechanisms of GAT1 inhibition, which involve a conformational change in the protein’s structure upon tiagabine binding, blocking the intracellular gate of the GABA release pathway. The highly detailed findings may unlock novel routes of GAT1 inhibition and iterative improvements upon current therapeutics for GABA-associated neurological disorders.
“These findings have direct implications on pharmacology as a whole, not only with respect to treating epilepsy, but many other diseases,” Gati added. “We have a feeling that this newly revealed mechanism is much more common than is currently thought, so we will investigate this first by using structurally similar inhibitors, and then expand our search to other molecules.”