Super-strength MRI identifies neurodegeneration in Parkinson’s disease
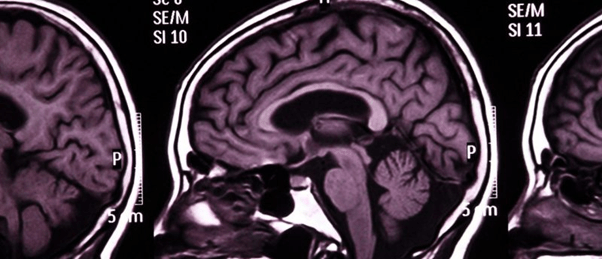
A novel, ultra-powerful MRI scanner helps to pinpoint Parkinson’s disease and identify patients who are most likely to benefit from new treatments.
Parkinson’s disease and similar conditions are associated with cognitive symptoms that are difficult to treat. In a recent publication, a research group from the University of Cambridge (UK) has used a high power MRI scanner at the Wolfson Brain Imaging Center (Cambridge, UK) to visualize the locus coeruleus – a noradrenaline-producing center of the brain that is associated with these cognitive symptoms – thus helping to identify patients who will benefit most from noradrenaline-boosting drugs.
Noradrenaline is a chemical that plays a key role in functions like attention, arousal, thinking and motivation. Non-motor symptoms in patients with Parkinson’s disease and similar conditions such as progressive supranuclear palsy (PSP) are thought to be related to a diminished supply of noradrenaline.
James Rowe, who led the study, explains: “Noradrenaline is very important for brain function. All of our brain’s supply comes from a tiny region at the back of the brain called the locus coeruleus – which means ‘the blue spot’. It’s a bit like two short sticks of spaghetti half an inch long: it’s thin, it’s small, and it’s tucked away at the very base of the brain in the brain stem.”
In PSP, experts believe that when noradrenaline breaks down it triggers a buildup of tau protein, which damages the cells that produce noradrenaline, leading to a continuous cycle that damages the locus coeruleus and diminishes noradrenaline levels. A similar process may occur in Parkinson’s disease.
 Is salt the key to accurate breast cancer diagnosis?
Is salt the key to accurate breast cancer diagnosis?
A new sodium MRI technique confirms that more active breast cancer tumors have higher salt levels, suggesting this could be used in diagnosis.
In a previous study by Rowe and his team, they examined donated brains and discovered that some people with PSP had lost as much as 90% of their locus coeruleus. In the present study, the team wanted to find a way to examine the locus coeruleus in living patients.
Most MRI scanners are 3T or below, which refers to the strength of their magnetic field, whilst the researchers of this study utilized a high strength 7T MRI scanner. This MRI scanner enabled the researchers to examine the locus coeruleus in patients with Parkinson’s disease and PSP and those in good health to identify any changes. Their results confirmed that higher levels of damage in the locus coeruleus region is linked to more severe symptoms of apathy and poorer performance on cognitive tests.
Thus far, MRI scanners have not been strong enough to measure this region in living patients. Impressively, the 7T MRI scanner can provide resolution at the size of a grain of sand, whilst most scanners can only provide detail at the level of a grain of rice.
Importantly, these results offer promise for treating cognitive symptoms, which can have a major impact on a patient’s outcome and wellbeing. A number of noradrenaline-boosting drugs have already been through clinical trials for other conditions, and Rowe and his team are currently leading a trial to see if these drugs will improve symptoms in PSP patients.
Noradrenaline boosting drugs would only benefit patients with damaged locus coeruleus, so having an MRI scanner that is able to identify this in patients is beneficial. “In the long term, this will prove more cost-effective than giving noradrenaline boosters to patients who ultimately would see no benefit,” says Rong Ye, the study’s joint first author.
“The ultra-powerful 7T scanner may help us identify those patients who we think will benefit the most. This will be important for the success of the clinical trial, and, if the drugs are effective, will mean we know which patients to give the treatment to,” concludes Ye.