Tuberous Sclerosis: to err is uniquely human

The complex process of human brain development plays an overlooked role in the manifestation of tuberous sclerosis, which leads to multiple noncancerous growths, previously thought to be solely due to genetic mutation.
Breakthrough research in cerebral organoids from Jürgen Knoblich’s lab at the Institute of Molecular Biotechnology of the Austrian Academy of Sciences (Vienna, Austria), has identified a cell type unique to human brains that is fundamental in the development of tuberous sclerosis. The findings dispute the current understanding that tuberous sclerosis is exclusively attributed to genetic mutation.
Tuberous sclerosis is a rare neurodevelopmental disorder characterized by non-cancerous growths or tubers in several areas including the brain, skin, eyes and kidney, manifesting in symptoms such as epilepsy, autism, learning difficulties and kidney problems.
The condition is attributed to genetic mutation in the TSC1 or TSC2 genes leading to decreased inhibition in mTOR signaling, which regulates cell proliferation, and the consequential dysregulation of cell growth and tuber formation. However, in previous studies of mouse models with mutations, the complete morphological and pathological changes witnessed in human brains with tuberous sclerosis were not all observed.
Researchers find evolutionary links between predator defense and REM sleep – the type of sleep associated with dreaming – in neural circuitry.
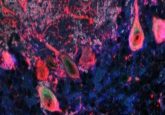
In an attempt to explain this gap in our understanding, Knoblich’s team generated cerebral organoids from people with TSC2 mutations to study tuberous sclerosis. The team utilized an in vitro human model, which allowed the analysis of features relating to tuberous sclerosis development that are unique to the human brain.
“Our findings on the root cause of tuberous sclerosis led us to a progenitor cell type specific to the human brain. This explains why the pathology of this disease could not be well established with other laboratory models,” explained Knoblich.
Knoblich’s team performed single-cell RNA-sequencing and histological validation of the organoid models, identifying a neural stem cell type unique to humans called caudal late interneuron progenitor (CLIP) cells.
The sensitivity of CLIP cells for mTOR signaling was determined to be ultimately responsible for the tuberous sclerosis instead of just genetic factors. When these CLIP cells proliferate in an unregulated manner it causes the development of tuber lesions. In addition, tuber formation occurred even with mutation in one copy of TSC2, with the second mutation occurring during tumor progression by copy-neutral loss of heterogeneity.
Epidermal Growth Factor Receptor (EGFR) signaling is required for CLIP cell proliferation and EGFR inhibition can revert the TSC phenotype, highlighting a prospective therapy for tuberous sclerosis to be investigated.
Whilst animal models can provide us with valuable insight into neurological mechanisms, the use of human-derived cerebral organoids, as demonstrated by Knoblich’s lab, are critical for acquiring an accurate understanding of the human brain and the neurological diseases that affect us.
“Our findings on human-specific principles in brain development and pathology could also apply to other known diseases for which no therapies exist to this date,” commented Knoblich “As a next step, we aim to investigate further neuropsychiatric diseases by adapting our technology further. We are confident that this human-derived laboratory model will finally help us identify human-specific mechanisms that have been overlooked for far too long!”