Sharing is caring: how bacteria transfer antibiotic-resistance genes
Extracellular appendages on gut bacteria accelerate the transfer of antibiotic-resistance genes.
“The death toll from antimicrobial resistance is expected to match cancer by 2050, meaning we urgently need new strategies to combat this trend,” commented Jonasz Patkowski (Imperial College London, UK), who is the first author of a recent paper studying how bacteria transfer genes. The international research team, led by researchers at Imperial College London, studied gut bacteria and revealed how extracellular appendages, called F-pili, might be behind the spread of antibiotic resistance among bacteria.
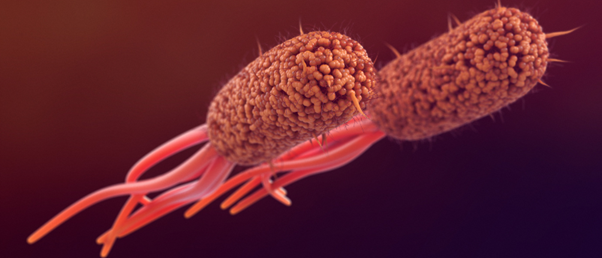
Bacterial conjugation is the process through which bacteria transfer genes and is a central mechanism behind the proliferation of antibiotic resistance. F-pili establish a connection between donor and recipient cells and are an essential part of this.
Previously, studies have assumed that F-pili would break in the harsh conditions found in the gut, thereby making the transfer of genes more difficult. A classic experiment seemed to show that they were so fragile that simply agitating the bacteria would break these extracellular appendages. However, if they are so fragile, why do so many bacteria found living in harsh conditions, like the gut, use this process to transfer genetic material?
 A new element in the fight against antibiotic resistance
A new element in the fight against antibiotic resistance
A novel method to biosynthesize fluorinated antibiotics has the potential to revolutionize antibiotic drug development.
The researchers wanted to test this assumption and started by shaking Escherichia coli bacteria during conjugation when F-pili were in use. They found that agitation did not break the appendages, and it actually increased the efficiency of the transfer of antibiotic-resistance genes. Additionally, after transferring genes, the agitated bacteria clumped together and formed biofilms more easily, which protects bacteria on the inside from any surrounding antibiotic molecules.
To investigate this further, the researchers used optical tweezers to pull at the F-pili on the bacterium to test its strength. The appendages revealed spring-like properties, which prevented them from breaking easily. They also subjected them to common gut conditions, including sodium hydroxide, urea and temperatures of 100°C; the F-pili remained intact throughout these conditions.
It’s known that F-pili are made of subunits that are linked by phospholipid molecules. The researchers used simulations to see how F-pili without phospholipids would behave when a force was applied with optical tweezers. They found they easily disintegrated, indicating that phospholipids are essential to the elasticity of F-pili.
“Making F-pili is very costly to the bacteria in terms of resources and energy, so it’s no surprise they are worth the effort,” explained Tiago Costa (Imperial College London), the senior author of the study. “We have shown how F-pili accelerate the spread of antibiotic resistance and biofilm formation in turbulent challenges, but the challenge now is to find ways to combat this very efficient process.”
Breaking or disrupting F-pili in pathogenic bacteria could be advantageous to prevent the spread of antibiotic resistance; however, finding ways to exploit their impressive properties and transfer mechanism could also be useful in drug delivery. Patkowski added, “It’s hard to find a tubular appendage with such strong properties. Bacteria use it to transfer genes, but if we could mimic these properties, we could use similar structures to precisely deliver drugs where they are needed in the body.”