Tailoring treatments for cancer with whole-genome sequencing
A new study lays the groundwork for a frameshift in treatment determination for several blood cancers; from karyotyping to whole-genome sequencing (WGS).
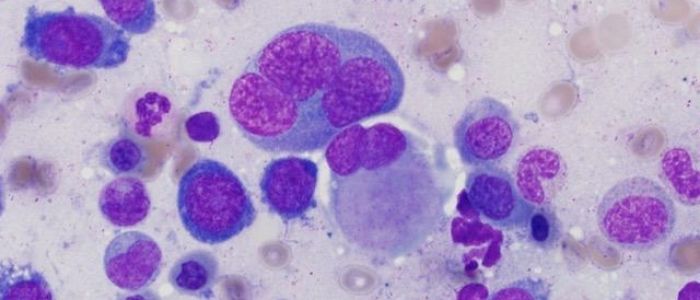
Recent research led by David Spencer of the McDonnell Genome Institute of Washington University (MO, USA) has highlighted the value of WGS to determine the optimal treatment course for patients with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS). The study provides a long-awaited update to the antiquated techniques currently used to determine treatment courses for patients with AML and MDS.
Patients with AML or MDS are typically divided into three risk categories that indicate their disease severity. These categories dictate the patient’s treatment strategy: ranging from chemotherapy-only for low-risk patients to high-priority bone marrow transplant and chemotherapy for those in the high-risk group.
The traditional process used to assign a patient to their risk group hinges on the process of karyotyping: using a microscope to examine a patient’s chromosomes in live cells to identify major genomic abnormalities. While additional single gene-sequencing tests of key genes have been bolted onto the process in recent years, this approach has remained largely unchanged for 30 years.
The rapid decline in the cost and time requirements of WGS has made the technique increasingly practical, and now cheap enough to cost a similar amount to conduct as traditional karyotypic and genetic testing.
To evaluate the practicality and performance of WGS, Spencer and his team used the tool to examine blood samples from 263 patients with AML or MDS. 117 of these patients were newly diagnosed, while the remainder were retrospective. The WGS results were then compared with results from traditional methods.
WGS successfully identified all of the major genomic abnormalities observed by karyotyping, alongside additional alterations in 17% of cases. Perhaps more poignant were the results in the newly diagnosed patients: here additional genetic abnormalities were observed in 25% of cases, leading to a change in risk category for 19 patients.
The cost of sequencing in this study equated to $1900 (USD) per patient, highly comparable to the $1000-2000 price range for the current standard. Furthermore, WGS was able to turn around results quickly, in an average of 5 days.
WGS is also less likely to provide an inconclusive result as it only requires a small sample of DNA from cancerous cells to conduct, while karyotyping requires a large number of live cells. These inconclusive results occur in 20% of AML and MDS patients, leading to delays in a patient beginning the appropriate treatment course.
While the team continues to investigate the utility of WGS for AML and MDS, the Siteman Cancer Center (MO, USA), from where the patients for the study were sourced, will now offer WGS to these patients.
Commenting on the study from an external perspective, head of the Wellcome Sanger Institute’s genome-sequencing studies, Pete Campbell, stated that “We stand on the threshold of an era in which we can identify every relevant genetic change in a given patient’s cancer in real time. This fascinating study demonstrates, first, that this technology can be implemented in real-world clinical practice, and second, that we can make more accurate choices of treatments for patients with blood cancers. Our task is now to take this blueprint for blood cancers and apply it to all cancers.”