Tumor-targeting protein could be future of personalized cancer therapy
A synthetic protein has demonstrated the ability to discriminate between cancerous and non-cancerous cells in vitro, showing potential for advances in personalized treatments.
Researchers from Stanford University School of Medicine (CA, USA) have engineered a system that can recognize the overly active biological pathways of cancer cells, killing them without affecting healthy surrounding tissue.
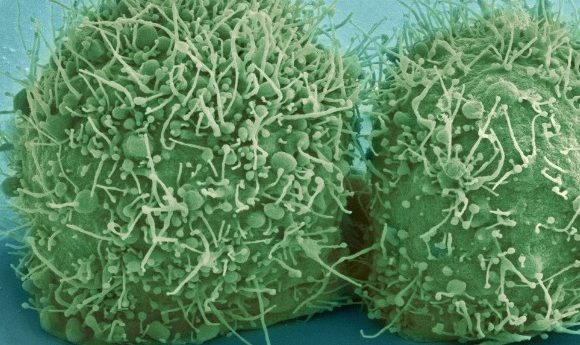
Signaling cascades are used in healthy cells for growth, development and recovery from injury. By responding to external triggers that bind to membrane receptors, these signals allow the cell to appropriately respond to its environment. In cancer these signaling pathways are disrupted and the receptor proteins of cancer cells can be overexpressed or mutated, fixed in an active state so that the cell has constant signals that stimulate growth. Two such receptors that can be affected are EGFR and HER2, both members of the ErbB family of receptors. These are often found in cases of brain, lung and breast cancers and are the target of many common anti-cancer drugs.
“The RASER approach could lead to a new form of personalized cancer therapy where treatment can be highly targeted and customized to the cancer type. ”
Receptor targeting drugs, such as Herceptin for breast cancer, are effective at blocking the growth signals, though lack the ability to discriminate between cancerous and non-cancerous cells, resulting in the death of both cells alike. “We haven’t had a drug that can tell the difference between a pathway signaling normally and one that is abnormally active,” commented senior author Michael Lin. “We knew we needed a better strategy, a more rational way of treating cancer. But we’ve not had a way to do it until recently.”
To overcome this issue, the group engineered a system for the “rewiring of aberrant signaling to effector release,” abbreviated to RASER. Relying on just two synthetic proteins, the RASER approach could lead to a new form of personalized cancer therapy where treatment can be highly targeted and customized to the cancer type.
The first synthetic protein, formed from two naturally-occurring proteins fused together, binds to activated ErbB receptors and cleaves a specific amino acid sequence. The second binds to the inner surface of the cell membrane and contains a customizable “cargo” sequence. This sequence performs a response programmed by the researcher, such as promoting the expression of genes that trigger apoptosis. When the first protein is bound to the active receptor, it cuts the second protein and releases its cargo into the cell.
-
Cancer, fruit flies and EGFR
-
Testing a blood test for lung cancer treatment
-
Improved preclinical drug studies with next-generation in vitro cancer models
“When the receptor protein is always on, as it is in cancer cells, the released cargo protein accumulates over time,” explained lead author Hokyung Chung. “Eventually enough accumulates to have an effect on the cell. In this way, the system produces an effect only in cancer cells, and we can convert the always-on state of the receptor into different outcomes through the choice of cargo protein.”
“We’re effectively rewiring the cancer cells to bring about an outcome of our choosing,” Lin added. “We’ve always searched for a way to kill cancer cells but not normal cells. Cancer cells arise from faulty signals that allow them to grow inappropriately, so we’ve hacked into cancer cells to redirect these faulty signals to something useful.”
The team compared the RASER system to two currently used breast cancer therapies, chemotherapy and a ErbB inhibitor, on a variety of in vitro cultured breast and lung cell types; cancerous with overactive ErbB, cancerous with normal ErbB activity and non-cancerous.
They found that, of the treatments tested, only RASER demonstrated specificity in killing cells with an overactive ErbB pathway. The traditional chemotherapy regime killed cells indiscriminately and the effect of the ErbB inhibitor varied though showed no correlation to pathway activity levels. Full results were recently published in Science.
Currently the RASER approach has only been demonstrated on cell culture and more work is needed to determine its viability as a treatment for human tumors in vivo. However, the team remain excited about the possible applications of the system, utilizing its customizability to recognize other mutated receptors and using different cargos to achieve different results.
Lin showed optimism about future studies and concluded with, “We have so much more information now about cancer genomics, signaling and how cancer cells interact with the immune system. It’s finally becoming practical to combine this knowledge with synthetic biology approaches to tackle some of these pressing human health problems. RASER is both customizable and generalizable, and it allows us for the first time to selectively target cancer cells while sparing normal signaling pathways.”